31 Oct Ocriplasmin Approved for VMT and Macular Holes
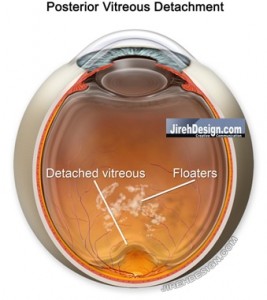
Posterior Vitreous Detachment “Separates” from the Retinal Surface
Ocriplasmin, or Jetrea, has been FDA approved. The drug is approved only for a retinal condition called vitreomacular traction (VMT) or vitreomacular adhesion (VMA). The VMT may or may not be associated with a macular hole.
What is VMT?
VMT is basically an incomplete, or partial, PVD (posterior vitreous detachment) with subsequent “pulling” on the macula. This “pulling” is also known as traction and can cause microscopic elevation on the macula and may lead to macular hole formation.
Ocriplasmin (previously known as microplasmin) may be an effective way to complete this PVD and chemically cleave the adhesion between the vitreous and macula.
Current treatment for vitreomacular traction and macular hole is surgical vitrectomy.
Intraocular Injection
Ocriplasmin is given as an intravitreal injection. The medicine is injected directly into the eye as are other intraocular injections of Avastin, Lucentis and Ozurdex.
Ocriplasmin is a proteolytic enzyme which may chemically cause a more complete separation of the vitreous and surface of the retina. Cleaving the adhesion between the vitreous and macular surface may improve vision and the macular hole, if present.
Results of Study
In the study presented to the FDA, patients received one injection of ocriplasmin.
- Jetrea caused resolution of VMT in about 26% of patients and caused a complete PVD in about 13%.
- Vision improved in a selected group; 25% of those with decreased vision of 20/50 or worse.
- Macular holes “closed” (i.e. fixed) in 40% of patients.
What Does This Mean?
This is a novel drug to chemically separate the vitreous from the retina. It has the potential to be an alternative to vitrectomy, the present accepted method for treating VMT and macular hole.
Intravitreal injections are delivered routinely in the office, thus, there is virtually no technique for physicians to “learn.”
The results, however, to not compare with the efficacy of vitrectomy eye surgery. VMT is “cured” almost all of the time and macular holes are repaired at least 90% of the time with a single surgical attempt.
We really don’t know if the safety of this particular injection is similar to other eye injections. Historically, other eye injections compare equally with vitrectomy with respect to intraocular infection and retinal detachment.
Lastly, for the floater community, I don’t believe this to be a substitute for surgery, but may be used as an adjunct to create a PVD before considering “floater only vitrectomy (FOV)”. Creating a PVD may make the floaters worse by changing the location +/- causing additional floaters.
As the use of Ocriplasmin becomes adopted by retinal physicians, it will be exciting to see if the efficacy of the drug can be improved and whether or not there will be other indications. For instance, will the results improve with repeated injections?

Matt Bullard
Posted at 12:30h, 31 OctoberWhat about the younger patients such as myself with floaters very close to the retina? Since a slight movement of floaters in this vicinity could mean a drastic improvement, would you be willing to test the drug in this manner, or is that even allowed?
Randall V. Wong, M.D.
Posted at 11:50h, 08 NovemberDear Matt,
When considering a vitrectomy, floaters close to the retina are not an issue. Proximity to the retina only seems to matter in the very, very few people who offer YAG laser for treatment of the floaters.
For now, without evidence of VMT/Macular hole, the drug can’t be reimbursed by the insurance companies…for now, that is.
My point has been that the rate of infection, as has been shown with all previous types of intraocular injections, has a higher rate of infection compared to vitrectomy.
So, you’ll have a safer and more effective procedure by vitrectomy.
To answer your question…yes, if you understand the risks, you could “test” the drug in this manner.
r
Jake Rashid
Posted at 13:06h, 31 Octoberwould this be something to trea a psuedo hole in th retina?
Thanks
Jake
Randall V. Wong, M.D.
Posted at 11:51h, 08 NovemberDear Jake,
Pseudo-hole is a specific appearing type of epiretinal membrane. According to the study, the ERM’s were resolved a small percentage of the time. Vitrectomy with removal of the ERM is almost 100%.
Randy
Darrell Farrier
Posted at 14:37h, 31 OctoberI just had a follow-up appointment with Dr. Wong for my retinal tear surgery. He continues to impress me with his understanding of eye issues and his personal treatment.
Randall V. Wong, M.D.
Posted at 00:19h, 09 NovemberDear Darrell,
Thanks so much for contributing!!!
This is very helpful to subsequent readers.
Many thanks,
r
Elena
Posted at 05:52h, 01 NovemberInteresting article as always.
I have a question: how can the separation of the vitreous from the retina “cure” PVD?
Can this drug help with the vitreous-retinal re-attachment?
It seems from the way you explain it in the article above that this drug (enzyme) makes a partial detachment complete. But then how do you avoid surgery for reattachment?
Randall V. Wong, M.D.
Posted at 00:37h, 09 NovemberElena,
Thanks for making a great point.
The enzyme, Ocriplasmin, may cause a PVD to occur, or, a partial PVD to completely separate faster than allowing Mother Nature take her course.
Retinal detachment is not the same as vitreous detachment. Bad choice of words and confusing.
Does this help?
r
Ken E.
Posted at 19:06h, 01 NovemberOnce again, a great article. Your view is consistent with everything I’ve read. I will be very interested to hear a first hand experience. Is this something you think ypu will pursue? Thanks Dr. Wong.
Randall V. Wong, M.D.
Posted at 00:46h, 09 NovemberHey Ken!
Not sure if this is going to fit into my practice philosophy. Not sure I understand why an injection is better than an operation. Certainly the cost differential is attractive, but the “success” rates are NOT comparable.
Great to hear from you. Thanks!
r
Elena
Posted at 07:52h, 06 Novembertesting — not sure what is going on with my posts
Randall V. Wong, M.D.
Posted at 12:26h, 11 NovemberElena,
They are up.
I have to approve each post (guarding against spam) before they are published. I try to answer post/comments weekly, sometimes longer.
Randy
Elena
Posted at 04:49h, 13 NovemberThanks, Randy.
Yes, that helps! Thanks to your many other articles here I know that vitreous detachment is not the same thing as retinal detachment and since you were referring to the vitreous detachment, it now makes sense.
And wow it sounds fantastic to be able to help the vitreous detach and possibly avoid tagging on the retina risking a real damage on the macula etc.!
Randall V. Wong, M.D.
Posted at 07:12h, 17 NovemberElena,
The drug really may have some use. We’ll have to see just how effective and widely it becomes adopted.
r
leslie
Posted at 14:38h, 16 Novemberwhen and where world wide will ocriplasmin be available first for doctors to give patients?
Randall V. Wong, M.D.
Posted at 07:30h, 17 NovemberDear Leslie,
I have no idea. This will be a decision for the manufacturer, Thrombogenics (thrombogenics.com).
Randy
floateredeyes
Posted at 22:22h, 22 NovemberHi Dr. Wong,
Is there a way to correlate anatomical retina with subjective visual field? We know that macula corresponds to our central vision (vision which has finer resolution and lets us read). What about peripheral retina? To how much into the periphery we can see?
I am asking this question because I want to correlate floaters in my vision to their anatomical location.
Regards
Randall V. Wong, M.D.
Posted at 21:26h, 03 DecemberDear Floateredeyes,
We usually see somewhere around 135-145 degrees out of each eye.
Helpful?
r
Elias
Posted at 17:41h, 09 DecemberDear Doctor Wong,
I’m 24 years old and have been suffering from floaters in both eyes for 5 years now, with symptoms getting worse (my vision is 20/20 otherwise). At this stage, the condition severely affects my ability to perform well in my job, drive cars, read or enjoy life in general. Eye doctors and a vitreoretinal specialist have suggested that I am too young for FOV given the risk of retinal detachment during surgery, and that I should wait “a few years”.
Would you – after consultation – in principle be able to offer FOV (with or without e.g. Jetrea/ocriplasmin pre-treatment) to someone at my age (24)? If yes, I would contact you to make an appointment. (insurance cover is not a concern for me)
Randall V. Wong, M.D.
Posted at 08:29h, 12 DecemberDear Elias,
I don’t agree.
Yes, after consultation, and if both you and I agree, vitrectomy might be possible.
I look forward to hearing from you.
Randy
Marie
Posted at 12:05h, 18 DecemberI’m 82 years old and have Vitreo Macular Traction in my right eye. I don’t mind that I can’t see well with that eye because my left eye does all the work. My eye doctor has me coming in every three months to see if it gets worse. I get the drops and pictures and it seems to stay the same. Is this checking procedure safe in your opinion?
Randall V. Wong, M.D.
Posted at 23:25h, 25 DecemberDear Marie,
The regular checkups with the drops and pictures is quite safe.
Keep checking.
Randy
Eric
Posted at 13:01h, 11 JanuaryHi Randy,
I’ll TRY to keep this short despite my complicated case! I appreciate your time and I hope you can answer my questions and possibly perform surgery on me.
1. I’m 42 yrs old and had a retinal tear & hole that was becoming a detachment in August. The episode started with a distinct flashing of light in lower left eye, out of the blue. Five hours later I was in the ER, and while the flashing stopped, every time I moved my eye a huge flash of light would appear in a crescent shape on left side of left eye. The ER doctor told me I was having a PVD, but no retinal detachment.
2. Over the month of August my eye filled with numerous floaters of different opacities, shapes, and sizes. I went back for two follow-ups and was told I had no detachment, despite the fact I absolutely knew something major was wrong. Then on Aug 31 my eye started to flood with hundreds of tiny black specks (in addition to the countless blobs and other larger floaters). I went back to the ER and was told I had a tear that needed immediate surgery.
3. I ended up with a full vitrectomy and scleral buckle on left eye. I am very happy with the surgery in that A) I can at least see with full peripheral 20/300 (i.e. not blind — it could have been much worse), B) I can see 20/25 with glasses (same as before detachment, I had LASIK on both eyes 8 yrs ago). However, the scleral buckle is squishing my left eye (thus resulting in the 20/300 vision), but it is also causing a dull pressure in my left eye & socket & muscles that is difficult to ignore.
QUESTION — Is it possible to loosen a scleral buckle to relieve some of this pressure/dull pain? Is it possible to completely remove the scleral buckle 6-12 months after surgery by assuming retina is fully re-attached and healed? I prefer the latter because I should also get my 20/25 vision back because the left eye will no longer be squished by the buckle. My eye is also very, very dry, probably due to the surgery — do you recommend Restasis?
4. Furthermore, for the past 4 months, my right eye (“good” eye) has been slowly filling with floaters (mostly sheet/blob type floaters, along with one distinct, dark, large floater that is the most problematic). In the past two months, the lower right corner of my right eye “flickers” like a flame almost continuously. It’s usually not quite bright enough to see during the day, but it’s visible at night.. I would say the flickering is present 75% of the time. This is _not_ an immediate onset/offset very bright flash like I had in my left eye; it’s a slowly building “flicker” that usually “on”.
QUESTION: I can literally feel a ‘tugging’ and ‘pinching’ in back of my right eye which I believe is due to VMA traction, would you agree, and would would an OCT scan be in order? The doctors tell me my retina is fine, and I’m probably not having a PVD either. How can this be?? The flickering light in lower right corner of right eye is worrisome to me.
5. My current problem is this: I work in software the combination of the floaters in the right eye (which are not only extremely annoying, but also cause blurred vision) and the dull pain in left eye (which is also blurry because it is so dry) are making it almost impossible for me to work on the computer and earn a living. Probably worse yet is that my driving is becoming impaired for similar reasons. I find that I’m moving my eyes so much during the day to relieve pressure on left eye and move right eye floaters out of the way, that (literally) my eye muscles are sore as if I was lifting weights with them! Something has to be done about this, and my doctor refuses to do a full vitrectomy or FOV. He also claims the Yag Laser floater doctors are quacks in it to make money — I find this ridiculous as I’ve researched the three doctors in US that do it, and I find them very reputable and honest.
QUESTION — This question has been asked 100’s of times before, but in my case where I’ve already had a detachment in the left eye, and my right eye has lattice degeneration (which was ‘reinforced’ by laser during the surgery on my left eye), would you recommend an initial treatment with laser to blast away the largest three floaters in my right eye and then see if I can live with the result? Or would you recommend that I head into your operating room and simply get the vitrectomy done? I would prefer to have a full vitrectomy, and if that means waiting until my right eye has a full PVD then I’m willing to do that. However, I have done a lot of reading on Ocriplasmin (JETREA) and it looks very promising in terms of inducing a PVD to allow a less risky vitrectomy. Does this agent also dissolve the floaters? If so, why not just avoid the surgery all together? Is there another agent in development that dissolves floaters (Vitrase)?
6. What is the recovery time for a floater vitrectomy? Is there a gas bubble involved? It took two weeks for my eye to recover enough after my vitrectomy + scleral buckle before I could see again, and another 1-2 weeks to have my vision stabilize so that I could work again with glasses on. Same deal here?
Thank you very much!
Eric
Randall V. Wong, M.D.
Posted at 18:39h, 22 JanuaryDear Zmonster,
Yes. Buckle only needed for 6-12 weeks after surgery in most cases, but can’t assume eye will regain same pre-operative shape and therefore the degree of near-sightedness. Can’t assume dull pain is related or due to the buckle. Restasis seems to work in most cases of dry eye, but can’t confirm that is your specific problem.
VM traction is painless. You can not feel it. Yes, OCT would be helpful to diagnose VMT. Flickering can be annoying and you are smart to get checked to make sure you don’t have a tear…especially given the history of the left eye.
Vitrectomy is best option. Ocriplasmin causes PVD <50% of the time. Vitrectomy not risky. Ocriplasmin does not dissolve floaters.
Vitrectomy (FOV) recovery is quick. Patch comes off and you start drops….easy. No gas bubble used nor needed. Vision should return within 24-48 of operation.
r
suzanne kauss
Posted at 16:00h, 13 JanuaryThank you for offering the updates.
Randall V. Wong, M.D.
Posted at 19:14h, 22 JanuaryDear Suzanne,
You are welcome!
r
Laurel Quinn
Posted at 20:27h, 22 JanuaryI’m wondering about the use of this drug in macular hole. Is the main mechanism of this drug inducing PVD? Would you say I would have to be pretty sure the patient did not already have a PVD to expect this drug to be effective for macular hole? Is it thought to release VMT in eyes that already have PVD? Do you know if these distinctions were looked at in studies and could you direct me to the references? THANK YOU!
Randall V. Wong, M.D.
Posted at 04:44h, 02 FebruaryDear Laurel,
I agree with you. Ocriplasmin may induce PVD, yet there is some improvement in cases where MH and VMT are apparent. The original article is a little difficult to sort out, but I agree with your argument. At this point, I don’t see why we need this, especially if surgical “cures” are much, much more successful.
Here is a press-release on FDA approval of Ocriplasmin.
r
Paul
Posted at 19:18h, 29 JanuaryWith ocriplasmin, do patients usually lie down for this procedure, or can they be seated upright? I assume that for vitrectomy patients would be lying down and aneathetised?
Randall V. Wong, M.D.
Posted at 05:11h, 02 FebruaryDear Paul,
Ocriplasmin is an injection…sitting down or lying is fine. I prefer patients lying as flat as possible for vitrectomy surgery.
r
motiram
Posted at 17:28h, 06 FebruaryMy mom is in her 60’s, diagnosed with VMT in OD. She already has Corneal Guttae.
She was asked to go thru vitrectomy and removal of cataract together. Is it safe to go thru that or use ocriplasmin. She is in India now, and I can check if ocriplasmin is available there, based on your suggestion. I would really really appreciate your response.
Randall V. Wong, M.D.
Posted at 12:20h, 13 FebruaryMotiram,
Answered this on other post.
r
motiram
Posted at 11:56h, 08 FebruaryMy mom is in her 60′s, diagnosed with VMT (macular hole) in OD. She already has Corneal Guttae.
She was asked to go thru vitrectomy and removal of cataract together. Is it safe to go thru that or use ocriplasmin. She is in India now, and I can check if ocriplasmin is available there, based on your suggestion. I would really really appreciate your response.
Randall V. Wong, M.D.
Posted at 12:18h, 13 FebruaryMotiram,
Sorry for the delay. I think vitrectomy and cataract surgery for macular hole is appropriate. Although Ocriplasmin is FDA approved, I don’t think it has a clear use, if ever. The results of successful macular hole closure with Ocriplasmin are nothing close to the success with vitrectomy.
Randy
pankaj yadav
Posted at 08:24h, 07 MayHello Doctor!
I am 22 yrs. old and having floaters in my both eyes from last 3 years. Just excited to know about vitreolase and vitreosolve to dissolve the floater.
My question is do you about this drug and till how much time it will take to come in the market?
Or there is any new drug for dissolving eye floater in the market is or research is going on ?
pankaj yadav
Randall V. Wong, M.D.
Posted at 18:36h, 12 MayDear Pankaj,
Jetrea may be similar to vitreolase (don’t know anything about this) in that it chemically causes a PVD.
It does NOT dissolve floaters.
Randy
Randall V. Wong, M.D.
Retina Specialist
Fairfax, Virginia
http://www.RetinaEyeDoctor.com
Paulie
Posted at 17:30h, 11 MayDear Randall,
I read these posts with great interest. After my hospital in England took a ‘watch and wait’ approach to my ‘stable VMT’ I have unfortunately developed a macular hole….I have been booked in to have a Vitrectomy but I am concerned that the registrar does not believe in posturing post-op describing it as voodoo….. I know this has been the topic of many papers but your comments on this would be greatly appreciated?
Many thanks,
Paulie
Randall V. Wong, M.D.
Posted at 18:56h, 12 MayDear Paulie,
I believe you are talking about face-down positioning after macular hole surgery.
I do agree that perhaps too much attention is spent on the positioning in that I believe the holes close within 1-2 days after surgery. In theory, if your doctor has put a sufficient amount of gas in your eye….positioning after surgery could be obsolete as there is always gas in contact with the macula.
On the other hand, face down positioning also decreases the time gas is touching the natural lens.
Randy
Randall V. Wong, M.D.
Retina Specialist
Fairfax, Virginia
http://www.RetinaEyeDoctor.com
Anne Akins
Posted at 19:48h, 10 DecemberDr Wong:
My mother is 82, has macular degeneration in one eye, and has developed vitreomacular adhesion in the other eye. She received a shot of Jetrea 6 weeks ago. 2 week follow-up showed a little improvement, and 4 weeks afterward, again minimal improvement, but the adhesion has not released.
Doctor suggested checking again in 2 weeks, just after the holidays, and said perhaps a 2nd injection should be tried. Everything I read says repeated injections are not recommended, can’t tell if it could be harmful, or just not enough study yet on that scenario. Any experience with this?
We are excited about the prospect of surgery, with her age, and the condition of her other eye, however we may be facing limited options.
thanks so much …..
Randall V. Wong, M.D.
Posted at 14:36h, 23 DecemberAnne,
If you had one choice, go for surgery with someone who is comfortable with ERM/VMT surgery. I’ve been underwhelmed with repeated doses of Jetrea.
Thanks and Happy Holidays!
Randy
Randall V. Wong, M.D.
Retina Specialist
Fairfax, VA 22030
http://www.TotalRetina.com
Brent Tuthill
Posted at 07:26h, 13 FebruaryI’m a 72 year old male, just diagnosed with VMT in the left eye. No macular hole was mentioned at the time of diagnosis a week ago. While the VMT incident occurred just before Christmas, I’d mistakenly assumed it was the first sign of macular degeneration (AMD), which I assumed I had – in the early stages – since the presence of drusen was mentioned during examination by optometrists for several years now. My current optometrist even
gave me an information sheet on macular degeneration at my last visit. And since I’d read that the appearance
of macular degeneration can be sudden, with symptoms similar to that of VMT, I just assumed it was AMD.
Unfortunately, I let it go, thinking that it was AMD and nothing could be done about it. Seven weeks passed before seeing an Ophthalmologist – when I got the surprising diagnosis of VMT; not AMD. If there had been any chance that the VMT would take care of itself, it would have already done so by this time, correct?
The retinal specialist I saw recommended Jetrea. However, he admitted that he’d done only 12 injections so far
and only 2 of them were successful. He did not define “success”.
It seems to me that Dr. Wong’s advise about going with a vitrectomy is the way to go, considering the lack of
success with Jetrea injection and any unidentified risks – either short term or long term – associated with using
this drug as an alternative to well established and generally successful surgery.
The only other question I have is – does the most up-to-date vitrectomy procedure still call for the face down
position for a week like I’ve been hearing so much about? Please tell me things have improved.
Thank you so much for all your help.
Randall V. Wong, M.D.
Posted at 11:24h, 16 FebruaryDear Brent,
I would agree that the vitrectomy is a better approach, both from a safety and efficacy standpoint. I am underwhelmed with the success of Jetrea.
I would pursue the possibility of a vitrectomy, but vitrectomy for VMT or epiretinal membranes DOES NOT REQUIRE GAS!!!!!
There for, no face down positioning! On the other hand, do you have a macular hole? It wasn’t clear in your comment.
Stay in touch.
Randy
Randall V. Wong, M.D.
Retina Specialist
Northern Virginia
Fairfax, VA. 22030
http://www.vitrectomyforfloaters.com
dg
Posted at 03:47h, 15 FebruaryDr. Wong,
I was recently diagnosed with a macular pseudo hole in my left eye. (In the same eye, three years ago I had laser surgery to repair a large retinal tear.) It was detected after a slight decrease in vision and via CT scan. The doctor recommends surgery.
I have been unable to find much information about the condition or the surgery. The doctor described it as attempting to pull tape off of something stuck to paper and hoping the paper doesn’t come off with it. Primitive but accurate? Is it a vitrectomy or different? In most cases, can the procedure result in no retinal detachment or gas bubble?
Many thanks in advance.
Randall V. Wong, M.D.
Posted at 11:56h, 16 Februarydg,
Pseudo-hole = epiretinal membrane (it’s just that the membrane creates the appearance of a macular hole, but there isn’t, hence “pseudo.”)
Here’s a video of ERM removal. It should be the exact same for pseudo-hole.
http://www.youtube.com/watch?v=2kTGM1fzohU
Randy
dg
Posted at 20:35h, 16 FebruaryThanks very much. Just a few questions:
1. Should progression be monitored by days, weeks, months or years? (I do retina checks every three months and was just diagnosed with the pseudo hole after a small drop in vision was recorded, and in horizontal lines I see small waves.)
2. I live in Japan. Do you know if surgical techniques here are as up to date as there? If not, I would consider going over to Fairfax . Or best to do the procedure close to where one lives?
Tks again.
Randall V. Wong, M.D.
Posted at 11:17h, 04 Marchdg,
If you’ve got a pseudo-hole, re-evaluation every few months is okay, but your doctor already recommended surgery, correct?
The procedure is very similar to peeling glue off the palm of your hand after drying. I’ll try and include a video of the operation….it is indeed a vitrectomy and, as such, usually does not require gas.
ERM/pseudoholes/macular holes can cause decreased vision and/or distortion.
http://www.youtube.com/watch?v=2kTGM1fzohU
Hope this is helpful. Would love to see you in Fairfax!
Randy
Randall V. Wong, M.D.
Retina Specialist
Northern Virginia
Fairfax, VA. 22030
http://www.vitrectomyforfloaters.com
Vickie
Posted at 17:03h, 07 MarchFace down and for how long after macular hole surgery?
Randall Wong, M.D.
Posted at 22:24h, 01 AprilIf you were my patient, about 5 days.
All the best and thanks for following.
Randy