10 Dec Sometimes You Just Need a Vitrectomy
A vitrectomy is an eye operation. It is performed by retina specialists for a variety of reasons. In patients with diabetic retinopathy, a vitrectomy may be useful to remove blood in the vitreous, aka a vitreous hemorrhage. There is no reason, to perform a vitrectomy in cases of macular degeneration.
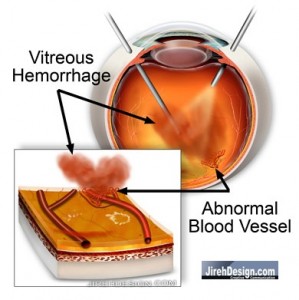
In cases of vitreous hemorrhage, bleeding has and blood remains suspended in the vitreous. The vitreous is the gel-like substance that fills most of the eye. It is very similar to jellyfish, it has substance, but is mostly water. It is optically clear.
A vitreous hemorrhage is benign, that is, the blood does not cause any damage to any portion of the eye, especially the retina. The vitreous hemorrhage physically blocks light and causes loss of vision. Sometimes the vitreous hemorrhage can absorb on its own, but if not, a vitrectomy is necessary to remove the non-clearing vitreous hemorrhage. At this point vision should be restored. It can take weeks or months to absorb. Many times we can’t wait that long.
Advanced diabetic retinopathy, or proliferative diabetic retinopathy, can have a retinal detachment associated with it. This type of retinal detachment is different. Most retinal detachments are caused by a retinal tear or retinal hole, called a “rhegmatogenous” retinal detachment.
Retinal detachments associated with diabetic retinopathy are called “traction” retinal detachments. The mechanism is different than rhegmatogenous retinal detachments in that the retina is pulled, like a tent, apart from the underlying layers. “Scar” tissue has formed on the surface of the retina, contracted and exerts this pulling.
A vitrectomy is necessary to correct/repair this type of retinal detachment. The vitreous is removed to allow access to the retinal surface. The abnormal scar tissue is cut away to relieve the “pulling.”
Vitrectomy surgery is also used for other retinal problems; rhegmatogenous retinal detachments, epiretinal membranes, macular holes, floaters, certain trauma, etc. Major risks of the surgery include blindness from infection and retinal detachment. The risks, however, are very, very uncommon.
Vitrectomy surgery has been around for about 30 years. It has allowed us to prevent potentially blinding retinal detachments in our diabetic retinopathy patients. On the other hand, the whole focus of this site is to educate. If you are seen early enough, you’ll never even need a vitrectomy.
“Randy”
Randall V. Wong, M.D.
Ophthalmologist, Retina Specialist
Fairfax Virginia

![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=f64d7fb7-9dd8-442e-b316-f59fa244de9d)
Donna Ramli
Posted at 23:40h, 17 DecemberMy husband has this syptoms, but he is not diabetics, can there be a cure without surgery? just with medicines (eyedrops or with eye balm?) as the eye is the most important part of the body and it scares him to have a surgery. His name is John Edwin Byrne and he is an American citizen. Thank you for responding
Randall V. Wong, M.D.
Posted at 04:48h, 18 DecemberThanks for your comment!
If your husband has floaters, they can be removed by surgery. A vitrectomy would be such an operation. Even though he is not diabetic, I’d make sure he doesn’t have some other cause for floaters or bleeding.
Has he been examined?
Randy
Donna Ramli
Posted at 05:59h, 18 DecemberYes, John has been examined, and his doctor suggest him to have a surgery. But it scared him and me too. Is it a minor surgery? what if he doesn’t take the surgery, what will happen to his eye? Please Sir, I really would appreciate if you can reply me on this. As John is in the U.S and I am in Indonesia, so I am a bit worried. What was the cause of his eye becoming like that? Can it be because he likes to work for hours in front of his computer everyday
Randall V. Wong, M.D.
Posted at 07:50h, 18 DecemberTry this link to my other site. It will describe vitrectomy surgery, etc.
He may also email me if he needs too.
Randy
Donna Ramli
Posted at 23:14h, 19 DecemberThank you very much Sir, but maybe you forgot that John is your patient. I had ask him if you were his eye doctor. And merry X-mas tou and your Family
mahwish
Posted at 09:46h, 17 Februaryhi,
My father had a glaucoma surgery two weeks ago. One of his stitches opened due to which he went for another surgery. Now he is suffereing from viterous hemorrhage. He’s a diabatic and hypertension patient. If the blood clots don’t settle down after two weeks, the doctor has recommended another surgery. Please let me know what are the risk factors if he goes through this surgery. How long is the recovery time period?
Randall V. Wong, M.D.
Posted at 07:52h, 18 FebruaryI am curious if the vitreous hemorrhage is from the glaucoma operation or from diabetic retinopathy. I would think it is from the glaucoma surgery. The blood may or may not clear in two weeks, but it is not doing any harm.
The risk factors for a vitrectomy are the same for any other intraocular surgery; blindness from infection and/or retinal detachment.
Depending on the surgeon and the techniques used; 25, 23 or 20 gauge systems, the “recovery” period is pretty quick. I hesitate giving you a firmer answer as I dont’ really know what you mean by “recovery” and I don’t know how bad the glaucoma has deteriorated the vision.
Good Luck!
Randy
Pingback:Risks of Eye Surgery
Posted at 13:15h, 17 April[…] operations such as cataract removal or vitrectomy. Cataracts are the most common eye surgery and vitrectomy eye surgery is usually performed by a retina specialist for various problems of the retina and vitreous. […]
Pingback:Optometry Student Observes Retinal Surgery
Posted at 08:02h, 21 April[…] “port of entry” to get into the retina. Before performing the laser, Dr Wong performed a “vitrectomy”. Vitreous is the jelly part of the eye, between the lens and the retina. It sort of keeps the […]
Pingback:How Retina Surgery is Performed
Posted at 06:21h, 26 April[…] Vitrectomy eye surgery involves minimal cutting on the eye. The use of 25-gauge instruments for vitrectomy eliminates cutting tissue on the outside of the eye, thus, there isn’t much discomfort any way. Scleral buckle surgery for retinal detachments creates the most discomfort due to increased cutting on the outside of the eye, but this method of anesthesia is still very effective. […]
james
Posted at 01:17h, 30 Augustmy mom diagnosed with damaged retinal vein and hemmorhage .doctor has fixed the surgery by 11th sep.please let me know whether she can travel by train after 5 days of surgery.her surgery is done through local anasthesia only
Randall V. Wong, M.D.
Posted at 09:51h, 30 AugustDear James,
I am not sure what is going on with your mother. Could you provide a more specific diagnosis and also the type of surgery she is having ? I should be better situated to answer your questions.
Randy
Peggyann Carnill
Posted at 14:34h, 31 MarchMY DAUGHTER, AGE 59 HAS HAD FLOATERS IN HER RIGHT EYE FOR 3 YEARS. HER DR. SAID NOTHING CAN BE DONE FOR THEM OTHER THAN DRASTIC SURGERY. NOW SHE HAS THEM IN HER LEFT EYE. I READ THAT A LASER TREATMENT IS AVAILABLE FOR THIS, HOWEVER I HAVE NOT LOCATED ANYONE WHO KNOWS ANYTHING ABOUT IT HERE IN ALTOONA, PA AREA. DO YOU KNOW OF ANY DOCTOR IN PA OR EVEN NEARBY STATES, I.E. MARYLAND, NEW YORK, WHO PERFORM THE LASER PROCEDURE? THANK YOU FOR YOUR HELP.
SINCERELY, PEGGYNN CARNILL
Randall V. Wong, M.D.
Posted at 07:41h, 07 AprilDear Peggyann,
Sorry for the delay, I was away for a few days for one of my kid’s hockey playoffs…a bit of a vacation, too.
Floaters can be removed with surgery. To many doctors, this may be viewed as drastic surgery, but for a retina specialist, a vitrectomy is quite routine.
You can not find a doctor locally to perform laser surgery for floaters because there are only 3 docs in the United States that perform such procedures. In my view, it is too risky compared to vitrectomy. The YAG laser is usually employed and, in my opinion, has too much potential for causing a retinal tear. Of the 3 docs, none are retinal specialists to my knowledge.
Risks of a vitrectomy are quite low and there are no published studies regarding the risk of laser used in this manner.
I hope this was helpful, I am biased in this area.
If I can help in anyway, please let me know.
Randy
Mark Sumimoto
Posted at 19:03h, 28 SeptemberMy Vitrectomy Experience with Dr. Wong
The experience began when I arrived at the Woodburn Surgery Center. It’s not the newest center, but the staff was warm and friendly. I was fitted with an IV and blanket. No undressing was required. They made everything as comfortable as possible.
Going into the surgery, I did not know exactly what to expect. I was laid back on a slightly negative incline beneath the laser machine. An oxygen line was put in my nose and a sedative was applied through the IV. There was a moment of panic when a wrap or mask was put over my head unannounced, but I cooled when I remembered I was breathing through the oxygen line. I asked if I was supposed to be groggy at this point, which was said to be an effect of the sedative. I do not know if any adjustments to my sedative were made, but I felt relatively alert as Dr. Wong went to work.
Though I know most of it was basically an optical illusion, what I saw from the inside was quite amazing. The needle entered my eye from the inner side, left side on my right eye. It was black against the background of bright light. I do not know if the needle was curved, but it appeared that way. The light, which I assume was white as I initially saw it, appeared to shift to different colors, blue, green, yellow and violet, as my retina tried to adjust. The swirled blood being removed by the needle was dark against it. I would compare it to deep space images of richly colored nebulas against the black background of space except reversed. I imagine seeing the needle taking the blood was like a hummingbird drinking nectar. I’d never seen anything like it before.
Despite being alert enough to see and remember all that, the procedure was free of lasting pain. The mechanisms holding my eye open were uncomfortable. More painful was the light shone into my eye. There was a somewhat dull pain when the needle entered my eye. It hurt, but was more of a focused muscle pain than a piercing one. Lastly, the laser itself did feel like it was burning my eye, which it was, but these were brief moments of discomfort. Afterwards, I felt as if someone had punched me in the eye, but no pain medication was needed.
While I wouldn’t call the experience enjoyable, overall, I’d say it was as close to it as the situation would allow, and I have no reservations about proceeding with the left one. (Edit: Left eye done. Went even more smoothly than right. Vision returned within a week.)
Randall V. Wong, M.D.
Posted at 19:29h, 28 SeptemberThanks Mark. You have done very well!
Thank you for sharing your experience with everyone!
Randy
Pingback:Alcon Constellation Vision System is the Best 25 Gauge Vitrectomy System
Posted at 16:47h, 14 July[…] best vitrectomy eye surgical system is the Constellation Vision System from […]
Pingback:Subconjunctival Hemorrhage Following Vitrectomy
Posted at 11:12h, 17 July[…] subconjunctival hemorrhage is quite frightening, but when following vitrectomy, it is quite […]