02 Aug The Timing of Retinal Detachment Surgery
There are 3 criteria I consider when deciding the timing of retinal detachment surgery;
- location of the retinal detachment
- duration of symptoms
- is central vision affected?
What Portion of the Retina is Detached?
By location, I don’t mean right versus left eye. At times the uppermost, or superior, portion of the retina is detached. These types of detachments usually enlarge faster than others. The fluid underneath the retina is affected by gravity and it is likely that gravity will influence superior detachments faster than others.
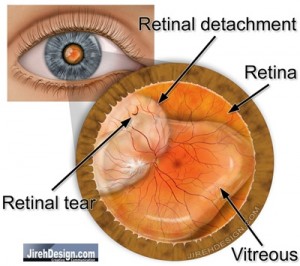
If the retinal detachment involves the uppermost (think of a clock, that part of the retina from 9 – 3 o’clock), then I am more likely to operate sooner than later. (In the illustration, the retina is detached from about 8 – 11 o’clock, the macula is attached).
How Long Has Vision Been Lost?
If symptoms of a retinal detachment have been present for a long time vs. just a few days, there is less of an “emergent” need to operate. For instance, if vision has been lost for weeks versus just a day or two, there is less of an urgency to schedule an eye operation. If symptoms have just begun, we might choose to operate sooner, say the next day.
On the other hand, sometimes a retinal detachment is so small, the patient doesn’t notice any problems. There is probably no urgency and we like to operate before symptoms develop.
Is the Macula Attached?
The most important criteria for operating emergently is the status of the macula.
What is the macula? The macula is the functional center of the retina. It provides our central vision. We use central vision to drive, watch TV, read, etc. In other words, our central vision is the most important and useful part of our “vision.”
Every attempt should be made to preserve the macula. I try to schedule surgery before the macula becomes detached.
The visual prognosis is decreased if the macula has become detached.
What Does This Mean?
Not every retinal detachment is an emergency. There is some urgency to most retinal detachments.
The most emergent situation arises when the macula is still attached, yet the superior retina (the area above the macula) is already detached. Gravity is almost certainly going to cause the macula to detach (maybe as soon as a day).
I generally try NOT to operate on an emergency basis. I guess what I really try to do is operate during normal business hours. During “after hours” the operating staff, patient and doctor are all stressed (no one wants to be there). This does not mean I don’t operate on weekends, most retinal specialists do …it’s part of your “deal.”
Most of the time, surgery can be scheduled within a few days time and can be done so to maximize your prognosis. Remember to consult your doctor.


Charles W Wetterling
Posted at 14:49h, 07 MayDear Dr. Wong, I just suffered a detached retina in my right eye. This is now my second eye to have a detached retina. In my first detached retinal operation, everything went very well, with essentially full recovery. However, with this latest detachment, I am experiencing something very upsetting. I just had this detachment within the last two weeks, and had a procedure performed within less than 24 hours. The issue that is upsetting and causing me great fear and anxiety, is that the eye shows everything slanted to the left approximately 5 degrees, so all vertical lines tilt to the left, and horizontal tilts left. This is especially upsetting, in part because I never had this occur after my left eye had it’s detachment. What would help me is to know if 1) This happens somewhat often or simply somewhat not so often, 2) does this most often go away, or not so often, and 3) what is it that causes this to happen. Sincerely, Charles
Randall V. Wong, M.D.
Posted at 15:27h, 13 MayDear Charles,
Hopefully this has resolved since your writing. There are so many causes for the distortion, I don’t want to alarm you unnecessarily.
I’d at least wait until the gas absorbs before worrying about the quality of the vision…that’s what I recommend to my own patients.
Also, make sure your doctor is aware of your symptoms.
r
Steve O Yang
Posted at 10:15h, 29 AugustDear Dr. Randall V. Wong,
I lost peripheral vision in the nasal inferior quadrant, but my central vision is still clear. Does this mean in my retina, the inferior nasal area is peeling off, or is it the complete opposite? I ask this, because I read somewhere that the image the retina sees is completely inverted before sending it to the brain.
Randall V. Wong, M.D.
Posted at 08:55h, 02 SeptemberDear Steve,
Everything is opposite. If your nasal inferior quadrant is detached, it should affect your temporal (temporal is opposite of nasal) and superior quadrant.
R